| Citation: | Wani Mudassir Maqbool, Durrani Abdul Munnan. Cost effective use of mosquito net mesh in inguinal hernia repair[J]. The Journal of Biomedical Research, 2019, 33(5): 351-356. DOI: 10.7555/JBR.33.20170138 |
Hernia repair is one of the most commonly performed operations in general surgery[1]. An ideal hernia repair should be durable and cost effective, producing low level of morbidity and allowing the patient to rapidly return to work or recreational pursuits. The modern age of hernia repair began in 1958, when American surgeon Usher et al[2– 3], described hernia repair using the Marlex mesh to provide a tension-free repair, which has become popular, due to its minimal invasiveness (local anesthesia, easy and reproducible technique, low recurrence rate, and low morbidity). Today, among the open techniques of inguinal hernia repair, the Lichtenstein repair is the most commonly used one[4]. There have been a lot of debates regarding the type of mesh used, with various materials being tried, such as stainless steel mesh, polyester cloth, nylon cloth, Dacron mesh, Teflon mesh, and Marlex mesh. The first generation of mesh was made of polyethylene, but difficult to sterilize because of its low melting point. In 1962, polypropylene mesh (PPM) was developed, satisfying all the requirements for an ideal mesh. Therefore, today it has become the best available material[5–6]. However, the limiting factor in the use of above meshes is their high cost.
Aiming at a direct comparison of the low cost mosquito net mesh (MNM) with the commercially available 20 PPM, we conducted a clinical randomized, double-blind study in inguinal hernia patients at the Shri Maharaja Hari Singh Hospital, Srinagar in Jammu and Kashmir, India. The primary endpoint was the efficacy and the secondary was cost effectiveness.
Patients
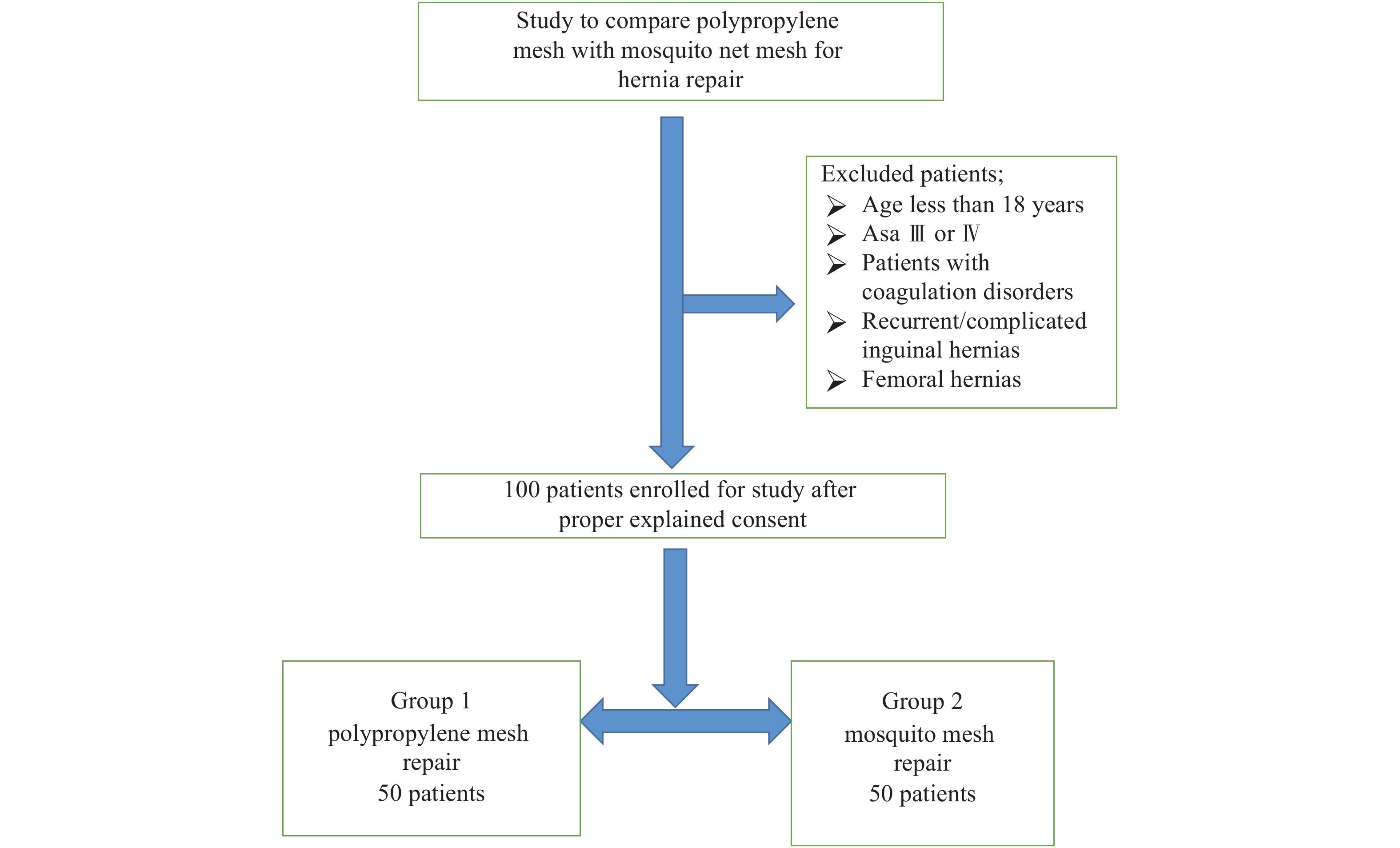
This clinical study was reviewed and approved by the Ethics Committee of the SMHS Hospital. Designed as a prospective, randomized, double-blind study and comprised of 100 patients with inguinal hernias admitted consecutively for elective surgery for groin hernia in various surgical wards of SMHS Hospital, from May 2011 to December 2012. Using the first generation randomization plan from the website www.randomization.com, we randomly divided the patients into two groups: Group 1, comprised of 50 patients underwent the polypropylene mesh repair (PMR) and Group 2, also containing fifty patients, underwent the mosquito net mesh repair (MMR). The study was approved by ethical committee of Applied Clinical Specialties of Govt. Medical College Srinagar. A written informed consent was taken from the patient or his/her guardian after fully explaining the nature of both the MNM and the PPM used for the repair in the language which they understood.
The patients were chosen unbiased from either sex and were above 18 years of age. High risk patients (ASA Ⅲ or Ⅳ), patients with coagulation disorders, recurrent/complicated inguinal hernias and femoral hernias were excluded from the present study (Fig. 1).
The patients were initially evaluated in the outpatient department on the basis of predetermined proforma and then admitted for surgery. Upon admission, detailed history was taken and general physical examination and systemic examination including local examination were conducted. Basic clinical blood chemistry and radiology were also performed. Pre-anesthetic checkup was done in all cases.
PPM: The PPM used in Group 1 was a commercially available. The mesh knitted monofilament, brought from a market, had the size of 7.5 cm×15.0 cm (Fig. 2).
MNM: The MNM used in Group 2 was the same as used in a previous trial in India[7]. The MNM was produced by Bangalore mono filament Pvt ltd (Fig. 3). The mesh was sterilized prior to use, and the quality was adequate with all quality assurance (QA) standards being met.
The surgery was performed as an as elective procedure. All mesh repairs were performed by a single certified surgeon (Associate Professor) of expertise in the Department of General Surgery, Government Medical College; Srinagar, India. Preoperative prophylactic antibiotics (Inj. Cefazolin 1 gm IV at the time of intubation). Meticulous part preparation with povidone iodine 10% was done and a mesh 7.5 cm×15.0 cm was used for the procedure tailored for each patient. All of the patients underwent Lichtenstein repair done under spinal anesthesia.
A 5 –6 cm skin incision was made, which started from the pubic tubercle and extended laterally within the Langer line. After the skin incision, the external oblique aponeurosis was opened and its lower leaf was freed from the spermatic cord. All steps of a standard Lichtenstein repair were carried out until placement of the mesh.
A sheet of 7.5 cm×15 cm of mesh, PPM in Group 1 and MNM in Group 2 was used (Fig. 4). The mesh was tailored to resemble the tracing of a footprint, with a medial sharper angle to fit into the angle between the inguinal ligament and the rectus sheath and a lateral wider angle to spread over the rectus sheath. With the cord retracted upward, the sharper corner was sutured with a non-absorbable monofilament suture material (1/0 Prolene) to the insertion of the rectus sheath to the pubic bone and overlapping the bone by 1 to 2 cm. This was a crucial step in the repair because failure to cover this bone with the mesh can result in recurrence of the hernia. The periosteum of the bone was avoided. This suture was continued (as a continuous suture with up to four passages) to attach the lower edge of the patch to the inguinal ligament up to a point just lateral to the internal ring. Suturing the mesh beyond this point was unnecessary and could injure the femoral nerve.
A slit was made at the lateral end of the mesh, creating two tails, a wide one (two-thirds) superior and a narrower one (one-third) inferior. The wider superior tail was grasped with forceps and passed toward the head of the patient from underneath the spermatic cord; this positioned the cord between the two tails of the mesh. The wider upper tail was crossed and placed over the narrower one and held with a hemostat. With the cord retracted downward and the upper leaf of the external oblique aponeurosis retracted upward, the upper edge of the patch was sutured in place with two interrupted absorbable sutures, one to the rectus sheath and the other to the internal oblique aponeurosis, just lateral to the internal ring using a single non-absorbable monofilament suture (1/0 Prolene). The lower edges of each of the two tails were fixed to the inguinal ligament just lateral to the completion knot of the lower running suture. This created a new internal ring made of mesh. The excess patch on the lateral side was trimmed, leaving at least 5 cm of mesh beyond the internal ring. Fixation of the tails of the mesh to the internal oblique muscle, lateral to the internal ring, was unnecessary and could have resulted in entrapment of the ilioinguinal nerve with the fixation suture. The external oblique aponeurosis was then closed over the cord with an absorbable suture (1/0 Vicryl). The skin was closed using 3/0 silk. Anti-septic dressing was applied.
The following parameters were recorded intra-operatively: Hernia characteristics like type of hernia whether indirect, direct, femoral, pantaloon, contents of sac, if any, size of mesh used were recorded based on intra-operative findings; Operative time was recorded from the time of incision to closure of the skin; Intra-operative complications, if any, were recorded.
After the operation, the patients were moved to a post-operative ward and monitored. Patients were usually discharged from the hospital on 1st or 2nd postoperative day in both groups. Post-operative hospital stay and complications, if any, was noted. After discharged, the patients were called for a follow-up at two weeks, two months, six months, one year, one and a half year and two years and results of surgery assessed. At the follow-up the patients were clinically examined for the appearance of seromas and hematomas, wound infection, testicular pain and swelling, chronic local pain and inguinal paraesthesia. Returning to normal (non-strenuous) work was encouraged and patient satisfaction with the procedure and recurrences, if any, were documented.
Data was expressed as average and as a percentage. All the inferences for inter group comparison was made by using non-parametric test measures. Yates corrected Chi square; Mann Whitney U test, Student's t-test and Odds ratio were applied for valid inferences as required. SPSS and MINITAB statistical packages were used. A P-value <0.05 was considered as significant.
The outcomes of the operation for the PMR and MMR group patients were compared. All patients and the observer (a certified general surgeon) were blinded. The same observer evaluated all of the patients before and after the operation during their follow-ups.
In our study the most common age groups were 41–50 and 51–60 years and highest incidence in the 4th and 5th decade showing that groin hernia was more common in the middle aged population. Minimum and maximum age of the patients were 23 and 80 years respectively, with a mean age of 50.53 years in all, 50.38 years in the MMR group and 50.68 years in the PMR group, showing that no age is exempted from this very common surgical problem (Table 1).
| Age (year) | MMR group | PMR group |
| ≤ 20 | 0 (0.0) | 0 (0.0) |
| 21−30 | 7 (14.0) | 6 (12.0) |
| 31−40 | 7 (14.0) | 9 (18.0) |
| 41−50 | 11 (22.0) | 10 (20.0) |
| 51−60 | 12 (24.0) | 10 (20.0) |
| 61−70 | 10 (20.0) | 13 (26.0) |
| 71−80 | 3 (6.0) | 2 (4.0) |
| Most common age groups in both the groups were 41−50 and 51−60 years. Minimum and maximum ages of the patient were 23 years and 80 years respectively. MMR: mosquito net mesh repair; PMR: polypropylene mesh repair. | ||
In our study, the presence of inguinal swelling alone was 60.0%, inguinal swelling associated with pain or in the form of dragging/pricking sensation was present in 40.0% of the cases (Table 2).
| Clinical presentation | Cases |
| Inguinal swelling alone | 60 (60.0) |
| Inguinal swelling with discomfort | 40 (40.0) |
In our study of 100 patients, majority of patients (82%) had an indirect inguinal hernia and 18% had a direct inguinal hernia. All of the bilateral hernias were direct.
In terms of site of hernia, we found that there was a definite right sided preponderance (60%) of cases, with left being (34%) and (6%) being bilateral. The bilateral cases were operated on one side only, the site decided by the surgeon as more symptomatic and the patient was assigned to only one group (Table 3).
| Type of hernia | MMR group | PMR group | ||||
| R | L | R | L | |||
| Indirect total | 28 (56.0) | 10 (20.0) | 26 (52.0) | 18 (36.0) | ||
| Direct total | 4 (8.0) | 4 (8.0) | 2 (4.0) | 2 (4.0) | ||
| Bilateral direct | 4 (8.0) | 2 (4.0) | ||||
| Total | 50 (100.0) | 50 (100.0) | ||||
| Total cases = 100. MMR: mosquito net mesh repair; PMR: polypropylene mesh repair; R: right; L: left. | ||||||
All of the patients were discharged from the hospital as soon as they became ambulant and tolerated orals. Patients in both groups were advised to exercise early ambulation. Orals were started as soon as when the post-operative nausea was over and the patient began to feel hungry, usually after 6 hours in patients who underwent general anesthesia, and as early as 1 –3 hours in patients with spinal anesthesia or local anesthesia. In our study the mean post-operative hospital stay was 1.22 days (range 1 –3 days) for the MMR and 1.20 (range 1 –3 days) for the PMR group, with no statistical significance between the groups (P>0.05). The overall mean post-operative hospital stay was 1.21 days (Table 4).
| Postoperative hospital stay (day) | MMR group | PMR group |
| 1 | 38 (76.0) | 39 (68.0) |
| 2 | 11 (22.0) | 10 (20.0) |
| 3 | 1 (2.0) | 1 (2.0) |
| Total | 50 (100.0) | 50 (100.0) |
| MMR: mosquito net mesh repair;PMR:polypropylene mesh repair. | ||
Complications
Wound infection: In the MMR group, four patients (8.0%) developed wound infection. In the PMR group, three patients (6.0%) developed wound infection. In no case the mesh was removed. It was classified as surgical site infection superficial type.
Wound seroma: In the MMR group, two patients (4.0%) developed wound seroma and in PMR, two patients (4.0%) developed wound seroma.
Wound hematoma: In the MMR group, one patient (2.0%) developed wound hematoma and in the PMR group, two patients (4.0%) developed a wound hematoma.
Urinary retention: In both groups, one patient (2.0%) had an episode of urinary retention which was managed by catheterization in the MMR group.
Chronic pain: One patient in each group developed persistent chronic pain in the inguinal region and were classified as chronic groin pain post hernia repair. Both were treated showed improvement during follow up.
Inguinal paresthesia: In the MMR group, one patient (2.0%) had inguinal paresthesia. Presently, he is undergoing follow-ups.
The patients were being followed up at intervals of two weeks, two months, six months, one year, one and a half year and two years. It was not seen in either groups in our study until December 2012.
The average time to return to work (non-strenuous) was 13.30 days in the MMR group and 13.68 days in the PMR group. Overall mean time to return to work was 13.49 days for both groups. There was no statistically significant difference between two groups.
The modern age of hernia repair began in 1958 when American surgeon Usher et al, described hernia repair using Marlex mesh to provide a tension-free repair that became popular due to its minimal invasiveness. Since then, Hernia surgery has got revolutionized. Mesh acts as "scaffolding" for new growth of a patient's own tissue, which eventually incorporates the mesh into the surrounding area. Mesh is used in both tension-free and laparoscopic tension-free hernia repairs. Mesh is generally available in various measurements and can often be cut to size.
In industrialized countries, alloplastic meshes are routinely used for hernia repair but in developing countries these are rarely available or affordable[7]. In India, the imported PPM is available and a 7.5 cm×15.0 cm mesh costs Rs 1 666/USD 36.22; the 15.0 cm×15.0 cm mesh costs Rs 3 724/USD 80.96, and the 30.0 cm×30.0 cm mesh costs Rs 9 430/USD 205[8]. In 1996, Indian surgeons found a polyethylene PPM, in the form of mosquito net mesh, a useful cost-effective alternative to standard meshes[8].
Clarke et al[9] in Ghana, reported the use of sterilized polyester PPM for inguinal hernia repair in 95 patients, using a total of 106 polyester PPMes. A trial in Burkina Faso which used a similar cheap nylon mosquito mesh has proven that there was no significant difference in the clinical short-term outcome of the hernia treatment or the surgeons comfort in handling the two different materials. Freudenberg et al, reported no severe complications while using the sterile nylon mosquito net versus the use of a commercial mesh for hernia repair in a randomized double-blind study in Burkina Faso.
Sanders et al revealed using vibrational spectroscopy that the material and mechanical properties of the polyethylene mosquito net are substantially equivalent to those of commonly used lightweight commercial meshes[10]. This study has revealed the macromolecular structure of the PPM. The mosquito net is a polyethylene homopolymer, knitted from monofilament fibers with a mean filament diameter of 109.7 μm and a mean mesh thickness of 480 μm. The mean pore maximum diameter is 1.9 mm, with 91.2% porosity, 53.7 g/m2 mean mesh weight, and a linear mass density of 152 denier. This is comparable to the "large pore" (class Ⅰ) commercial meshes. The bursting force for polyethylene mosquito net is greater than for UltraPro and Vypro (43.0 N/cm vs. 35.5 N/cm and 27.2 N/cm, respectively), and the mosquito net exhibited less anisotropy compared to the commercial meshes[11].
Another recent study has revealed that in vitro infection risk of using the polyethylene mosquito net is not significantly different from commonly used monofilament polypropylene commercial prosthetics and is in fact lower than a commonly used commercial multifilament mesh. This study adds to the growing body of evidence that indicates that these meshes can be safely deployed[12].
Thus it could be concluded that the cheap indigenous PPM which has similar properties of an imported mesh can be safely used for tension-free inguinal hernia repair in adults and without any additional financial burden to the patient and should be considered the standard of care for treating inguinal hernias, especially, in the poor patients who cannot afford the imported PPM. Further trials with a larger number of patients and longer follow-ups are justified and recommended.
| [1] |
Levard H, Boudet MJ, Hennet H, et al. Inguinal hernia repair: a prospective multicentre trial on 1706 hernias[J]. Br J Surg, 1996, 83(Suppl2): 72.
|
| [2] |
Usher FC. Further observations on the use of marlex mesh: a new technique for the repair of inguinal hernias[J]. Am Surg, 1959, 25: 792–795.
|
| [3] |
Usher FC. Hernia repair with knitted polypropylene mesh[J]. Surg Gynecol Obstet, 1963, 117: 239–240.
|
| [4] |
Lichtenstein IL, Shulman AG, Amid PK, et al. The tension-free hernioplasty[J]. Am J Surg, 1989, 157(2): 188–193. doi: 10.1016/0002-9610(89)90526-6
|
| [5] |
Amid PK, Shulman AG, Lichtenstein IL. The Lichtenstein open "tension-free" mesh repair of inguinal hernias[J]. Surg Today, 1995, 25(7): 619–625. doi: 10.1007/BF00311436
|
| [6] |
Ortiz-Oshiro E, Villalta GC, Furió-Bacete V, et al. Non-absorbable prosthetic meshes: which is the best option in the repair of abdominal wall defects?[J]. Int Surg, 1999, 84(3): 246–250.
|
| [7] |
Tongaonkar RR, Reddy BV, Mehta VK, et al. Preliminary multi centric trial of cheap indigenous mosquito-net cloth for tension-free hernia repair[J]. Indian J Surg, 2003, 65: 89–95.
|
| [8] |
Wilhelm TJ, Freudenberg S, Jonas E, et al. Sterilized mosquito net versus commercial mesh for hernia repair. an experimental study in goats in Mbarara/Uganda[J]. Eur Surg Res, 2007, 39(5): 312–317.
|
| [9] |
Clarke MG, Oppong C, Simmermacher R, et al. The use of sterilised polyester mosquito net mesh for inguinal hernia repair in Ghana[J]. Hernia, 2009, 13(2): 155–159. doi: 10.1007/s10029-008-0460-3
|
| [10] |
Freudenberg S, Sano D, Ouangré E, et al. Commercial mesh versus Nylon mosquito net for hernia repair. A randomized double-blind study in Burkina Faso[J]. World J Surg, 2006, 30(10): 1784–1789, 1790. doi: 10.1007/s00268-006-0108-3
|
| [11] |
Sanders DL, Kingsnorth AN, Stephenson BM. Mosquito net mesh for abdominal wall hernioplasty: a comparison of material characteristics with commercial prosthetics[J]. World J Surg, 2013, 37(4): 737–745. doi: 10.1007/s00268-012-1900-x
|
| [12] |
Sanders DL, Kingsnorth AN, Moate R, et al. An in vitro study assessing the infection risk of low-cost polyethylene mosquito net compared with commercial hernia prosthetics[J]. J Surg Res, 2013, 183(2): e31–e37. doi: 10.1016/j.jss.2013.01.047
|
| Age (year) | MMR group | PMR group |
| ≤ 20 | 0 (0.0) | 0 (0.0) |
| 21−30 | 7 (14.0) | 6 (12.0) |
| 31−40 | 7 (14.0) | 9 (18.0) |
| 41−50 | 11 (22.0) | 10 (20.0) |
| 51−60 | 12 (24.0) | 10 (20.0) |
| 61−70 | 10 (20.0) | 13 (26.0) |
| 71−80 | 3 (6.0) | 2 (4.0) |
| Most common age groups in both the groups were 41−50 and 51−60 years. Minimum and maximum ages of the patient were 23 years and 80 years respectively. MMR: mosquito net mesh repair; PMR: polypropylene mesh repair. | ||
| Clinical presentation | Cases |
| Inguinal swelling alone | 60 (60.0) |
| Inguinal swelling with discomfort | 40 (40.0) |
| Type of hernia | MMR group | PMR group | ||||
| R | L | R | L | |||
| Indirect total | 28 (56.0) | 10 (20.0) | 26 (52.0) | 18 (36.0) | ||
| Direct total | 4 (8.0) | 4 (8.0) | 2 (4.0) | 2 (4.0) | ||
| Bilateral direct | 4 (8.0) | 2 (4.0) | ||||
| Total | 50 (100.0) | 50 (100.0) | ||||
| Total cases = 100. MMR: mosquito net mesh repair; PMR: polypropylene mesh repair; R: right; L: left. | ||||||
| Postoperative hospital stay (day) | MMR group | PMR group |
| 1 | 38 (76.0) | 39 (68.0) |
| 2 | 11 (22.0) | 10 (20.0) |
| 3 | 1 (2.0) | 1 (2.0) |
| Total | 50 (100.0) | 50 (100.0) |
| MMR: mosquito net mesh repair;PMR:polypropylene mesh repair. | ||